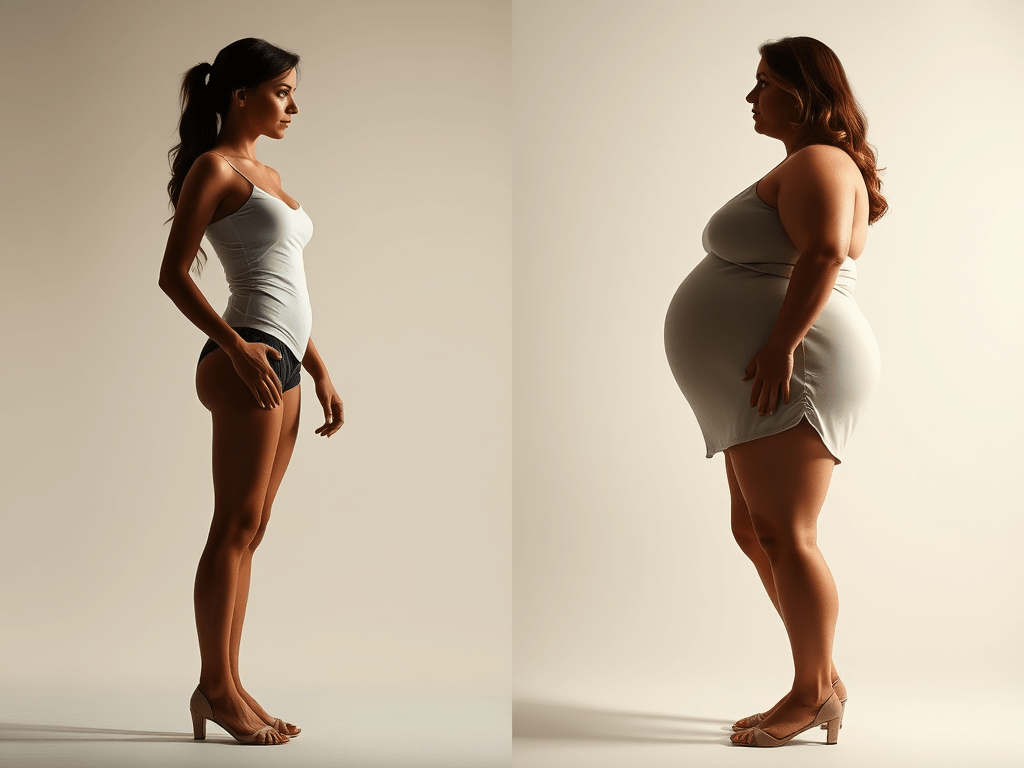
For some, gaining even a single kilogram feels impossible. For others, the kilos arrive so fast they barely recognize themselves. Sudden weight loss or gain isn’t just about food — it’s biology, life events, and mental health colliding. This guide names the causes, cuts through harmful “quick fixes,” and offers a safe, realistic path forward.
Two Sides of the Same Struggle
- Unexplained weight loss: low appetite, early fullness, fatigue, anxiety about hidden illness. Often tied to depression, overactive thyroid, GI issues or major stress.
- Sudden weight gain: swelling appetite, cravings, low energy, shame. Common with cortisol surges, hypothyroid, insomnia, medications, or emotional eating.
Both the “too thin” and the “plus-size” body face judgment. Both may be battling real medical and emotional drivers you can’t see.
Biology You Can’t See (But Feel Every Day)
- Cortisol (stress hormone): long work hours, financial strain, caregiving, or grief raise cortisol → more hunger, belly fat storage, slower metabolism. In some people, stress suppresses appetite and weight drops.
- Thyroid, sex hormones, insulin, leptin/ghrelin: imbalances can amplify gain or block regain after loss.
- Medications: antidepressants, antipsychotics, steroids, hormones, some diabetes or seizure meds can shift weight up or down.
- Long surgery or illness: anesthesia, inflammation, bed rest, antibiotics, and low intake cause muscle loss and appetite shutdown; rebuilding takes structured rehab.
Life Events That Reshape the Body
- Pregnancy & Postpartum: normal gain, then sleep deprivation + prolactin/estrogen shifts + stress → stubborn fat retention. Appetite or supply anxiety can also drive undereating.
- Menopause & the “after-period” years: lower estrogen slows metabolism and redistributes fat to the waist.
- Divorce, grief, workplace burnout: appetite swings (loss or overeating), erratic routines, skipped meals, late-night snacking.
- Social media pressure: before/after culture fuels extremes, crash diets, and shame.
- Genetics: some bodies store fat easily; others struggle to keep it. Comparisons are unfair by design.
Why Weight Doesn’t “Bounce Back”
- Metabolic adaptation: after rapid loss, your body defends a lower burn rate.
- Muscle loss: illness, surgery, long bed rest, or extreme diets reduce lean mass → slower metabolism.
- Sleep debt & stress load: keep cortisol high and hunger signals noisy.
- Gut and appetite signaling: illness, antibiotics, or chronic stress can blunt hunger or increase cravings.
The Hidden Danger: “DIY Fixes” That Harm
Please avoid:
- Unregulated pills/teas/supplements promising fast loss or rapid gain.
- Medication without prescription: thyroid drugs, hormones, diuretics, laxatives, steroids.
- Crash diets / extreme fasting / over-exercise right after illness, surgery, childbirth, or during depression.
- Stacking stimulants, “detoxes,” or appetite suppressants with mental-health meds.
These can injure your heart, hormones, liver, and mood — and usually backfire.
A Real Problem-Solving Plan
1) Safety First — When to See a Doctor
- Unintentional change ≥5% of body weight in 3–6 months (up or down).
- Ongoing loss of appetite, persistent nausea/diarrhea/constipation, night sweats/fever, palpitations, hair loss, or new swelling.
- Post-surgery: weight still falling or strength not improving after 4–6 weeks.
Ask for: CBC, thyroid panel, iron/B12/Vit D, fasting glucose/A1c, lipids, CRP, and any tests your symptoms suggest.
2) If You’re Losing Weight and Struggling to Regain
- Structured meals: 3 meals + 2 snacks at consistent times. Don’t wait for hunger; use the clock.
- Calorie target: gentle surplus (~+300–500 kcal/day). Prioritize protein 1.2–1.6 g/kg, healthy fats (olive oil, nuts, avocado), and easy extras (powdered milk in soups, olive oil on grains).
- Liquid nutrition: smoothies, milk/yogurt drinks if solids are hard.
- Light resistance training 2–3×/week (bands/bodyweight) to rebuild muscle and appetite.
- Post-surgery add-ons: protein at each meal, short walks 3–5×/day, gradual step goals, and a dietitian if appetite is absent after 2–3 weeks.
- Depression-linked loss: pair nutrition plan with therapy; eating gets easier as mood stabilizes.
3) If You’ve Gained Suddenly and Feel Stuck
- Calorie approach: modest deficit (–300–500 kcal/day), never extreme.
- Protein first (1.6–2.2 g/kg) to control hunger and protect muscle.
- Fiber 25–35 g/day (veg, legumes, whole grains) and hydration to blunt cravings.
- 10–15-minute walks after meals to aid blood sugar control.
- NEAT (non-exercise movement): standing tasks, stairs, stretching breaks each hour.
- Sleep & stress: 7–9 hours, fixed sleep/wake times; a simple wind-down routine to drop cortisol.
- Medication review: ask your clinician if a weight-neutral alternative exists.
4) Postpartum, Menopause, and the “After-Period” Years
- Postpartum: avoid crash diets. Pair protein-forward meals with stroller walks; 2 short strength sessions/week. Ask for help with sleep — recovery accelerates with rest.
- Menopause/perimenopause: priority is muscle maintenance (2–3 resistance sessions/week), protein at each meal, and consistent sleep. Expect slower loss; aim for steadiness, not speed.
5) Workplace, Social Media, and Divorce/Grief Realities
- Work: pack protein + fiber; schedule a non-negotiable 10-minute walk after lunch. Caffeine curfew 2 pm.
- Social media: unfollow “before/after” accounts that trigger extremes. Track behaviors, not just weight (meals, steps, sleep).
- Divorce/grief: appetite chaos is normal. Use meal templates (e.g., soup + grain + protein) and set alarms to eat. Therapy is not optional; it’s treatment.
6) Weekly Structure That Works (Repeat for 4–6 Weeks)
- Mon–Fri: same breakfast and lunch template; 10–15-minute post-meal walks; 2–3 short strength sessions (20–30 min).
- Sat: shop and batch-prep 2 proteins, 1 grain, 1 tray of vegetables.
- Sun: review energy, mood, sleep, and adjust one variable (bedtime, steps, protein).
What To Be Careful Of (Quick List)
- Drastic plans that promise results in days.
- Skipping medical evaluation when weight changes are sudden or unexplained.
- Mixing supplements/“fat burners” with prescription meds.
- Training hard on too little protein or sleep — it preserves fatigue, not health.
- Comparing your body to someone else’s highlight reel.
Building a Healthier Perspective
Health isn’t a single number. It’s steady energy, recoverable strength, stable mood, and routines you can live with.
Key Takeaways
- Sudden weight change is a signal, not a cosmetic issue — often linked to stress, depression, hormones, or recovery from surgery/illness.
- Common triggers: cortisol (stress), thyroid or sex hormones, medications, pregnancy, postpartum, menopause, grief, workplace burnout, and genetics.
- Why it doesn’t “bounce back”: metabolic slowdown, muscle loss, sleep debt, and appetite signaling changes.
- Avoid quick fixes: crash diets, unregulated supplements, or self-medicating with hormones or pills — these often worsen the problem.
- Safe next steps:
- Get a medical check-up to rule out hidden conditions.
- Focus on consistent, balanced meals and protein.
- Use light resistance training to rebuild muscle.
- Prioritize sleep, hydration, and stress management.
- Seek therapy or counseling when depression, grief, or anxiety are drivers.
- Redefine success: it’s not about chasing your old weight or social media ideals, but about restoring strength, stability, and long-term health.
Conclusion
Behind every body — thinner than expected or carrying extra weight — is a real story of biology, life events, and resilience. The way back is not through punishment or risky shortcuts, but clear diagnosis, patient habits, muscle rebuilding, better sleep, and mental-health care. Give your body time; give yourself compassion.
Read More from Curianic
- How Work and Lifestyle Pressure Trigger Different Types of Depression — why stress and daily routines can quietly reshape both mood and body.
- Burnout vs. Deep Fatigue: What Modern Wellness Often Misses — the hidden difference that explains why rest alone doesn’t fix exhaustion.
- Work Stress Is Destroying Your Sleep: How to Escape, Recover, and Take Back Your Life — how broken sleep fuels cortisol, cravings, and weight shifts.
- When Everything Feels Cloudy: Brain Fog, Vision Haze, and the Echoes We Rarely Talk About — the cognitive toll of lifestyle imbalance that often pairs with physical changes.