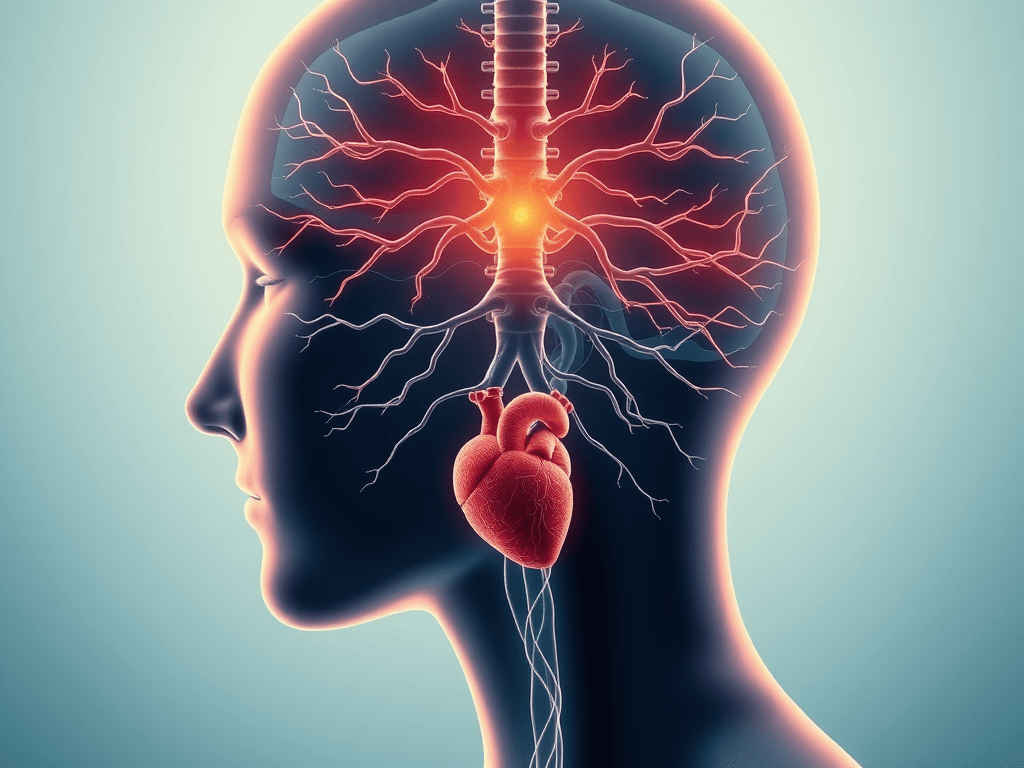
The vagus nerve is rarely mentioned in everyday medical conversations, yet it quietly governs some of the body’s most essential functions: heart rhythm, digestion, breathing, immune balance, and the ability to recover from stress.
Known anatomically as the tenth cranial nerve, the vagus nerve forms the main communication highway between the brain and vital organs. When it functions well, the body knows how to calm itself. When it does not, stress becomes chronic, digestion falters, and recovery slows.
Understanding the vagus nerve is not about trends or wellness shortcuts. It is about understanding how the human body regulates safety, balance, and repair.
What Is the Vagus Nerve?
The vagus nerve is the longest and most complex cranial nerve in the human body. It originates in the brainstem and extends downward through the neck into the chest and abdomen.
Along its path, it connects directly to:
- The heart
- The lungs
- The stomach
- The intestines
- The liver
- The spleen
Because of this extensive reach, the vagus nerve acts as a biological messenger, continuously informing the brain about the internal state of the body.
The Autonomic Nervous System and Balance
The autonomic nervous system has two primary branches:
- Sympathetic system: activates fight-or-flight responses (stress, alertness, survival)
- Parasympathetic system: supports rest, digestion, immune repair, and recovery
The vagus nerve is the primary driver of the parasympathetic system.
Its role is not to eliminate stress, but to tell the body when danger has passed and it is safe to slow down.
Why the Vagus Nerve Matters More Than We Think
When vagal function is healthy, the body:
- Regulates heart rate efficiently
- Maintains steady breathing patterns
- Digests food effectively
- Controls inflammation
- Recovers from psychological stress
- Transitions smoothly between effort and rest
When vagal signaling is weak or disrupted, the nervous system can remain locked in survival mode, even when no threat exists.
Common Signs of Low Vagal Tone
Low vagal tone is not a diagnosis, but a pattern often observed in people exposed to prolonged stress or trauma.
Common associations include:
- Chronic anxiety or constant alertness
- Digestive issues (bloating, IBS-like symptoms, nausea)
- Heart palpitations or irregular rhythm
- Shallow breathing
- Fatigue and poor sleep
- Sensitivity to stress or noise
- Difficulty relaxing, even during rest
These symptoms often appear together because they share a common regulatory pathway.
The Gut–Brain Axis: Where the Vagus Nerve Dominates
Approximately 80% of vagal signals travel from the body to the brain, not the other way around. This means the brain relies heavily on feedback from the gut and organs to decide how safe the body is.
This explains why:
- Digestive health strongly affects mood
- Chronic gut issues increase anxiety
- Stress alters appetite and digestion
The vagus nerve is the biological bridge connecting emotional states with physical regulation.
The Vagus Nerve and Constipation: When Digestion Slows Down
Constipation is often discussed in terms of diet, hydration, or bowel anatomy. However, in many cases, laboratory tests and imaging show no clear structural cause. When this happens, the problem is frequently regulatory rather than mechanical — and the vagus nerve plays a central role.
The vagus nerve is a key regulator of gastrointestinal motility. Under normal conditions, it supports the rhythmic contractions of the intestines (peristalsis), stimulates digestive secretions, and signals when elimination can occur safely.
When vagal activity is reduced, intestinal movement slows. Stool transit time increases, water absorption continues, and constipation develops — often accompanied by bloating, gas, and abdominal discomfort.
Why Stress-Related Constipation Is So Common
Chronic stress shifts the nervous system toward a persistent sympathetic (“fight-or-flight”) state. In this mode, digestion becomes a low priority. Vagal signaling decreases, and the parasympathetic support necessary for bowel movement is suppressed.
Importantly, this mechanism explains why many people experience:
- Constipation during prolonged psychological stress
- Digestive improvement during vacations or periods of emotional safety
- Recurrent constipation despite normal medical tests
In these cases, the intestines themselves may be healthy, but their neural regulation is disrupted.
The Gut–Brain Feedback Loop
Because most vagal signals travel from the gut to the brain, impaired digestive signaling can reinforce stress responses. This creates a feedback loop in which constipation and nervous system dysregulation sustain one another.
This interaction helps explain why constipation often coexists with:
- Anxiety disorders
- Sleep disturbances
- Pelvic floor tension
- Hormonal sensitivity
- Chronic fatigue
None of these patterns imply that symptoms are psychological. They reflect the biology of prolonged nervous system imbalance.
Stress, Trauma, and Vagal Shutdown
Acute stress activates the sympathetic system temporarily, which is normal.
Chronic stress, however, reduces vagal signaling, keeps the body in defensive mode, and prevents full physiological recovery.
Over time, this may affect immune balance, hormonal regulation, digestion, and reproductive health. This response represents biological adaptation, not personal weakness.
Supporting Digestive and Nervous System Regulation
In cases where structural, hormonal, or metabolic causes have been ruled out, restoring vagal tone may become an important part of management.
Evidence-based supports include:
- Slow diaphragmatic breathing with extended exhalation
- Gentle vocalization (humming or singing)
- Exposure to cool air or water on the face
- Rhythmic walking
- Mindful movement
- Predictable daily routines
These approaches do not replace medical treatment, but they address a regulatory dimension that conventional approaches often overlook.
Conclusion
The vagus nerve highlights a fundamental truth of human biology: health depends not only on organs and chemistry, but on regulation.
Digestive disorders, stress-related symptoms, and functional constipation often share a common pathway — the nervous system’s ability to recognize safety and shift into repair mode.
Understanding this connection allows for a more integrated and compassionate view of health.
Read More from CURIANIC
- When Stress Feels Physical: How Hormonal Burnout Locks the Body Into Survival Mode
- Tired But Wired: How Cortisol Imbalance Is Wrecking Your Sleep and Focus
- Invisible Inflammation: The Hidden Cause of Fatigue, Brain Fog, and Weight Gain
- Low Iron, High Impact: Why Women’s Fatigue Is Often Misdiagnosed
- Burnout vs. Deep Fatigue: What Modern Wellness Often Misses
- The Mental Load No One Talks About: How Decision Fatigue Is Stealing Your Energy
- When Everything Feels Cloudy: Brain Fog, Vision Haze, and the Echoes We Rarely Talk About